 Health
Health
 Spine
Spine
 Symptoms - Cause
Symptoms - Cause
Don's Home
 Health
Health
 Spine
Spine
 Symptoms - Cause Symptoms - Cause
|
Under Construction 
Contents: Symptoms | Causes | Diagnosis |Terms/Glossary | Books | Articles | Treatment This is an overview of back problems collected from books and web sites; It has not been reviewed by medical professionals and is not a substitute for advice from a healthcare professional. Experts tend to have a variety of opinions on causes and solutions for back pain and we have not attempted to rate them on level of agreement. Second opinions are strongly recommended.
About 80 percent of the adults in the U.S. have been bothered by back pain at some point. Lower back pain (LBP) is the fifth most common reason people go to a doctor. Low back pain is second only to the common cold as a cause of lost days at work.
Symptoms: Warning signs that may indicate a problem that needs IMMEDIATE EVALUATION:
Causes: There are generally two causes Musculoskeletal, which account for 2/3 to 3/4 of back pain, and neurological (pinched nerve). The simplest cause is a muscle sprain or ligament sprain. These can last from six to eight weeks, but usually improves over time. A combination can occur when nerve irritation causes muscle spasms or swollen muscle tissue pushes against a nerve.
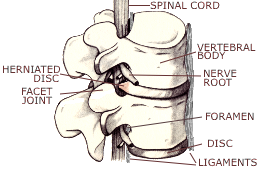
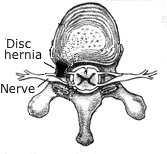
Radiculopathy - A pinched nerve due to a herniated disc. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 See Vertebrae muscles and ligaments on the illustration page. |
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Degenerative lumbar scoliosis or curvature of the spine typically develops in individuals over 50 years and may be caused by asymmetric degeneration of the spine. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
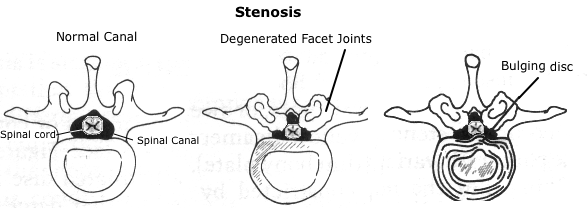 Central or spinal stenosis - A narrowing of the spinal canal, which can compress sensory nerve fibers causing loss of sensation. Acquired stenosis usually is related to older age and results from the thickening of the facet joints due to disc degeneration, disc space narrowing, and excess bone deposits.
Central or spinal stenosis - A narrowing of the spinal canal, which can compress sensory nerve fibers causing loss of sensation. Acquired stenosis usually is related to older age and results from the thickening of the facet joints due to disc degeneration, disc space narrowing, and excess bone deposits.See: Questions & Answers about Spinal Stenosis at The National Institute of Arthritis and Musculoskeletal and Skin Disease (NIAMS) in the National Institutes of Health (NIH) Natural History of Lumbar Spinal Stenosis at SpinalStenosis.org Cervical spondylotic myelopathy (compression of the spinal cord in the cervical area) from cervical stenosis, caused by degeneration of the disk or vertebrae. It is the most common cause of spinal cord disfunction amongst people older than 55. It usually causes neck, arm and shoulder problems (pain or numbness or pins-and-needles) because those nerves are closer to the surface of the spinal cord in the cervical area, but it may also cause bladder problems and/or cause weakness or jerky movement in the legs. Foraminal stenosis - Bone spur into neural foramen putting pressure on nerve root.
Facet joint problems - When facet joints become worn or torn the cartilage may become thin or disappear and there may be a reaction of the bone of the joint underneath producing osteoarthritis, overgrowth of bone spurs and an enlargement of the joints. Lumbar spondylolisthesis (LS) - One of the spine bones slips forward over the one below it. As the bone slips forward, the nearby tissues and nerves may become irritated and painful. Sacroiliac Joint (SI Joint) Pain is caused by problems in the connection between the sacrum (tailbone) and hip.
Other Causes:
Many intra-abdominal disorders-such as appendicitis, aneurysms, kidney diseases, bladder infections, pelvic infections, and ovarian disorders, among others-can cause pain referred to the back.
Depression, Stress and other emotional issues are frequently associated with back pain. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Distribution of spinal nerve roots and associated muscles The vertebrae are numbered from top to bottom: Cervical - C1-7; Thoracic - T1-12; Lumbar - L1-5, Sacral - S1-5 (fused) and Coccyx (4 fused).
The spinal cord fills 95% of the spinal column at the cervical vertebrae, but only 60% in the lumbar. The heart, lungs, gastrointestinal tract and most other organs are connected to the vagus nerve which extends through the through the neck near the thorax and not the spinal cord.
Effects of Spinal Injury:
Source: The Merck Manual of Medical Information - Home Edition reprinted in: June 1999 Newsletter of the National Centre for Classification in Health at Univ. of Sidney. and Cervical Radiculopathy at eMedicine Sports Medicine Cervical radiculopathy is a dysfunction of a nerve root of the cervical spine. Cervical radiculopathy occurs at a much lower frequency than radiculopathy of the lumbar spine. The annual incidence is approximately 85 cases per 100,000 population.
Lower Back Nerves
The sensory (cutaneous) nerves leave the spinal cord in the dorsal root (posterior root) and the motor (muscle) leave in the ventral root (anterior root).
The Femoral Nerve arises from nerve fibers from the the L2-L3-L4 portion of the lumbar spine. The Femoral Nerve then passes down the inside edge of the thigh, past the inside of the knee and towards the ankle and foot.
It is rare for sciatic nerve roots other than L4 and L5 to be damaged by lumbar disc herniation.
The symptoms of damage to nerve L5 are:-
Leg weakness can be caused by spinal stenosis in a cervical vertebrae (C5-8) putting pressure on a nerve which runs all the way down to the legs, but it is usually associated with arm or shoulder problems because these nerves are closer to the edge of the spinal cord there. 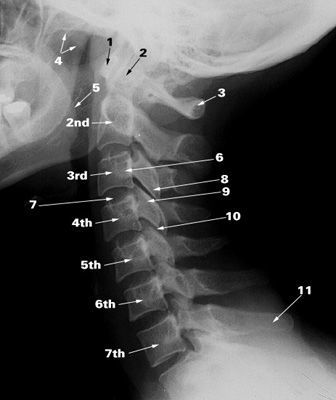 Cervical vertebrae (C1-7)
Cervical vertebrae (C1-7)
1. Anterior arch of the atlas (C1) 2. Dens (odontoid peg around which atlas rotates) of axis (C2) 3. Posterior arch of the atlas (C1) 4. Soft palate (roof of the moutn) 5. Root of the tongue 6. Transverse process 7. Intervertebral disc 8. Inferior articular process 9. Superior articular process 10. Zygapophyseal (facet) joint 11. Spinous process of C7 2nd-7th: The bodies of 2nd to 7th cervical vertebraeSource: University of Szeged, Hungary | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Diagnosis: A computed tomography (CT or CAT) scan or magnetic resonance imaging (MRI) study is usually performed to confirm the associated condition and best procedure. Studies between 1998 and 2000 and an article in the Journal of the American Medical claim that MRIs resulted in more surgeries with no better outcome.
An Electromyogram (EMG) is often performed when patients have unexplained muscle weakness. The EMG helps to distinguish between muscle conditions in which the problem begins in the muscle and muscle weakness due to nerve disorders. EMGs can also be used to isolate the level of nerve irritation or injury.
Nerve conduction studies (NCS) are frequently done at the same time as an EMG. A shock-emitting electrode is placed directly over the nerve and a recording electrode is placed over the muscles under control of that nerve. Several quick electrical pulses are given to the nerve, and the time it takes for the muscle to contract in response to the electrical pulse is recorded. Anesthetic injections can be made at different locations to pinpoint the source of pain. e.g. nerve root blocks or faces blocks. Myelogram: a liquid dye is injected into the spinal column. The dye circulates around the spinal cord and spinal nerves, which appear as white objects against bone on an x-ray film. A myelogram can show pressure on the spinal cord or nerves from herniated disks, bone spurs, or tumors. See: Diagnosis of Spinal Stenosis at U. Washington Treatment see the treatment page
Surgery:
Orthopedic surgeons specializing in spine surgery and neurosurgeons can
treat disc herniations, disc degenerations, spinal stenosis and fractures of the spine, slippage of the spine (spondylolisthesis), scoliosis, bone tumors of the spine. Only neurosurgeons are trained to perform procedures inside the lining of the spinal canal. Scoliosis and other spinal deformities are still primarily treated surgically by orthopedic spine specialists.
Fusion: The goal of the lumbar fusion is to have the two vertebrae fuse (grow solidly together) so that there is no longer any motion between them after a Discectomy.
The most common type is a posterior lumbar interbody fusion (PLIF) . During an interbody fusion, the surgeon removes the intervertebral disc (discectomy) and places either a piece of bone or a metal or plastic cage in its place.
Posterior lumbar interbody fusion (PLIF) is a type of spinal fusion procedure that utilize a posterior (back area incision) approach to fuse (mend) the lumbar spine bones together (using an interbody fusion technique). Interbody fusion means the intervertebral disc is removed and replaced with a bone spacer (metal or plastic may also be used), in this case using a posterior approach. The posterior technique is often favored when one or two spinal levels are being fused in conjunction with a posterior decompression (laminectomy) and instrumentation (use of metal screws/rods).
In many cases metal frames are attached to the bones or rods are screwed into vertebrae to hold them steady while the fusion occurs.
Spinal Fusion - Minimally invasive lumbar spinal fusion is an operation that is less invasive to the traditional lumbar spinal fusion to treat degenerative disc disease and other vertebral problems. There are advantages and disadvantages to the procedure.
The Swedish Lumbar Spine Study Group compared 3 methods of fusion in 222 patients with physical therapy in 72 patients. It showed, that pain was reduced by 33% in the surgical group compared to 7% in the controls and disability was reduced by 25% compared to 6% in controls. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Lumbar Interspinous Process Decompression (IPD) , also known as interspinous distraction or posterior spinal distraction, has been proposed as a minimally invasive alternative to laminectomy and fusion. In IPD an interspinous distraction implant, also called a spacer, is inserted between the spinous processes through a small (4-8 cm) incision. The supraspinous ligament is maintained and assists in holding the implant in place. No laminotomy, laminectomy or foraminotomy is performed. The device is intended to restrict painful motion while enabling otherwise normal motion. The device theoretically enlarges the neural foramen, decompresses the cauda equina and acts as a spacer between the spinous processes to maintain the flexion of the spinal interspace.
Discectomy
Spinal fusion may or may not be done in conjunction with a discectomy.
Partial Discectomy
Laminoplasty
Posterior Dynamic Stabilization System is a dynamic stabilized device with the emphasis on motion preservation of vertebrae; it's a flexible frame with metal screws and rods placed from the back into the bonesframe simulating a healthy spine to support the body physically. Fixed (non flexible) rods may also be used to stabilize the back after fusion or to straighten a curvature of the spine. They may be attached with screws into the vertebral body or hooks over the lamina. Osteophytes (bone spurs) can be ground off.
Other Minimally invasive procedures:
Nucleoplasty - Use of hot wires or lasers to evaporate disk material. IDET (Intradiscal Electro-Thermal Annuloplasty/Coagulation) - A probe inserted into the disc to heat the tissues. Pain reduction may occur through the thermal coagulation of nociceptors in the outer annulus. PIRFT (percutaneous intradiscal radiofrequency thermocoagulation) - Similar to IDET, but uses radiofrequency energy. It is thought to reduce the nocioceptive pain input from the free nerve ending in the outer anulus fibrosis.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Terms/Glossary: ACDF - Anterior cervical discectomy and fusion. EMG - Electromyogram - Test of muscle reaction CAT scan - computed tomography - Produced by a special x-ray machine connected to a computer to produce cross-sectional images. Cauda Equina Syndrome - A serious neurological problem due to pressure from a disc on the lower portion of the spinal cord and spinal nerve roots. CBT - Cognitive-behavioral therapy CBLP - chronic back and leg pain Cervical spondylotic myelopathy - compression of the spinal cord in the cervical area CSF - Cerebrospinal fluid CT scan - same as CAT scan Discectomy - Removal of all or a portion of the disc material. A partial Discectomy removes a fragment of a disc that is causing the pressure on the nerve. Sometimes all of the nucleus pulposus is removed to prevent risk of further prolapse, Discogram/Discography - A radio-opaque dye is injected into the disk; an X-Ray is then taken to view the disc anatomy and to see if the dye leaks out of the disc. Epidural - An injection of Steroid or Anesthetic in epidural space between the bony ring of the spine and the covering of the spine called the dura. See image. DC - Doctor of Chiropractic - 2-4 years of college plus 4 years of a chiropractic college course, and a 1 year internship. Chiropractic colleges are accredited by the Council on Chiropractic Education. recognized by the U.S. Department Education. D.O. - Osteopathic physician - 4 years of college plus 4 years of curriculum as well as internship and residency training similar to a M.D. They are licensed to practice medicine, perform surgery, and prescribe medication. D.O.s receive extra training in the musculoskeletal system. E Stim - (also E Stem) Electronic Muscle Stimulation ESI Epidural steroid injections Fusion Surgery causing two vertebrae to fuse (grow solidly together) so that there is no longer any motion between them. Herniated Disk - A disk that slips out of place or ruptures. Also called a Bulging disk, Compressed disk, Herniated intervertebral disk, Herniated nucleus pulposus, Prolapsed disk, Ruptured disk, or Slipped disk. These terms are all are used differently by doctors. FAAP - Fellow in the American Academy of Pediatrics IDET (Intradiscal Electro-Thermal Annuloplasty/Coagulation) - A probe inserted into the disc to heat the tissues. Pain reduction may occur through the thermal coagulation of nociceptors in the outer annulus. Laminectomy - Removal of a section of the bony covering over the back of the spinal . Laminotomy - Only a portion of the lamina is cut and extracted. LS - Lumbar spondylolisthesis - Caused when one vertebrae slips forward. MRI - magnetic resonance imaging MIS - minimally invasive spine surgery Myelopathy - The gradual loss of nerve function caused by disorders of the spine. Neurologist - Treats problems like seizures, Parkinson's disease, headaches, tremor, and peripheral nerve problems like numbness and burning. Neurosurgeon - Treats brain and spine problems. Those specializing in spine surgery can perform procedures inside the lining of the spinal canal. NCS - Nerve conduction studies NCV - nerve conduction velocity NSAID - Nonsteroidal anti-inflammatory medications (e.g. aspirin, ibuprofen, Naproxen) nucleus pulposus - jelly-like substance in the center of a disc. OMT (osteopathic manipulation) - Manipulation performed by an Osteopath (DO) Orthopedic surgeons perform bone and joint surgery, however some specialize in spine surgery and treat disc herniations, disc degenerations, spinal stenosis and fractures of the spine. osteopathic manipulative medicine (OMM) Osteoarthritis - The cartilage around a joint wears out and causes the joint to rub against each other, creating inflammation and pain. Can be any joint not just vertebra. The most common form of arthritis. Osteomyelitis - Vertebral osteomyelitis is the infection of the bones of the vertebral column. It may be caused by either a bacteria or a fungus. Bacterial or pyogenic vertebral osteomyelitis is the most common form. Osteophytes - Bone Spurs Osteoporosis - Reduced bone density OT - Occupational Therapist PCEA- patient controlled epidural analgesia, see epidural Physiatrists - rehabilitation physicians P.T. - Physical Therapist PIRFT (percutaneous intradiscal radiofrequency thermocoagulation) - Similar to IDET, but uses radiofrequency energy. It is thought to reduce the nocioceptive pain input from the free nerve ending in the outer anulus fibrosis. PLIF - Posterior lumbar interbody fusion - A graft placed between the vertebral bodies PNT (Percutaneous neuromodulation therapy) - Treatment for pain by electrical stimulation directly to the deeper tissues (muscles, ligaments, tendons) near the spine through several needle electrodes. Prolapsed Disc - See Herniated disc Prolotherapy - Injection (often containing a sugar solution, which is an irritant) into the ligaments or tendons, which causes irritation, but stimulates repair and the growth. Radiculopathy - A pinched nerve due to a herniated disc. Sciatica - Pain running down the leg from pressure on the Sciatic nerve SCS - Spinal cord stimulation SNRB - Selective nerve root block Spondylosis - Osteoarthritis Spondylolisthesis is a condition in which a bone (vertebra) in the lower part of the spine slips forward and onto a bone below it. Stim - See E Stim Subluxation - Misalignment of the spinal column. Chiropractic subluxation is usually too minor to see on an x-ray. Traditional chiropractic subluxation theory claims that spinal adjustments can solve problems such asthma, digestive problems, etc in addition to back pain. Orthopedic subluxation is a partial dislocation of a bone in a joint causing pain and limiting range of motion. Subligamentous disk herniations are contained by the posterior longitudinal ligament. Supraligamentous disk herniations not contained by the posterior longitudinal ligament. This is also called transligamentous herniation or disc extrusion. TENS - Transcutaneous electrical nerve stimulation TLIF - Transforaminal lumbar interbody fusion TMS - Tension Myositis Syndrome - Psychosomatic causes of backpain Made popular by Dr. Sarno's bestseller "Healing Back Pain: The Mind-Body Connection" Vertebral subluxation - See subluxation. Vertebroplasty: A minimally invasive procedure in which a bone cement is injected into the spine in order to relieve the pain from certain spine fractures. Whiplash - A injury to the soft tissues that hold the cervical vertebrae together (ligaments, facet capsules, muscles), typically from a rear-end car accident. It can cause pain or weakness in the arm or hand as nerves are squeezed. Zygapophyseal - Facet joint on the back of the vertebrae.See: Glossary at spine-health.com Spinal Surgery Glossary by Stanton Schiffer M.D. at the Western Neurosurgical Clinic Back and Leg Pain - Definition List at NYU
Books: "Do your really need back surgery", by Aaron Filler, 2004 Your Aching Back: A Doctor's Guide to Relief, by Augustus A. White III, MD, 1990 The Truth About Back Pain: A Revolutionary, Individualized Approach to Diagnosing and Healing Back Pain by Todd Sinett, DC & Sheldon Sinett, DC, 2008 (DC - Doctor of Chiropractic) Back Pain: How to Relieve Low Back Pain and Sciatica by Carol Ardman, Loren Fishman MD, 1997 Do You Really Need Back Surgery?: A Surgeon's Guide to Back and Neck Pain and How to Choose Your Treatment, by Aaron G. Filler M.D., 2004 The Mindbody Prescription: Healing the Body, Healing the Pain, by John E. Sarno M.D., 1998 A followup to his 1990 best selling book "Healing Back Pain: The Mind-Body Connection" Straight-talk, No-nonsense Guide to Back Care, 1984, The AMA, Consumers Union
Articles:
Links: This website also contains material copyrighted © by 3rd parties. Medical Multimedia Group (MMG), LLC (incl. eOrthopod.com); Consumers Union; Medscape.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||