|
Sinusitis is infection or inflammation of the lining of the sinus cavities. These are hollow spaces in your cheeks and around your eyes. Sinus infections often follow a cold and cause pain and pressure in your head and face.
Sinusitis can be either acute (sudden) or chronic (long-term). With chronic sinusitis, the infection or inflammation does not completely go away for 8 weeks or more.
What causes sinusitis?
Sinusitis can be caused by three things:
- Viruses.
- Bacteria.
- Fungi.
The same viruses that cause the common cold cause most cases of sinusitis.
When the lining of the sinus cavities gets inflamed from a viral infection like a cold, it swells. This is viral sinusitis. The swelling can block the normal drainage of fluid from the sinuses into the nose and throat. If the fluid cannot drain and builds up over time, bacteria or fungi (plural of fungus) may start to grow in it. These bacterial or fungal infections can cause more swelling and pain. They are more likely to last longer, get worse with time, and become chronic.
Postnasal Drip:
The excess mucus production that triggers postnasal drip has a number of possible causes, including:
- Colds
- Flu
- Allergies (called allergic postnasal drip)
- Sinus infection or sinusitis (inflammation of the sinuses)
- Object stuck in the nose (more common in children)
- Pregnancy
- Certain medications (including some birth control pills and blood pressure medications)
- Deviated septum (abnormal placement of the wall that separates the two nostrils) or another anatomical problem that affects the sinuses
- Changing weather fronts, cold temperatures, or excess dryness in the air
- Certain foods (for example, spicy foods may trigger mucus flow)
- Fumes from chemicals, perfumes, cleaning products, smoke, or other irritants
Sometimes the problem is not that you're producing too much mucus, but rather that it's not being cleared away effectively. Swallowing problems can cause a buildup of liquids in the throat, which can feel like postnasal drip. These problems can sometimes occur with age, a blockage, or conditions such as gastroesophageal reflux disease (GERD).
Prilosec is frequently prescribed. There are others.
Source: Postnasal Drip: Causes, Treatments, Symptoms, and More
See also 3-Step Silent Reflux Prevention Plan | The Dr. Oz Show
Tooth infections and Sinus
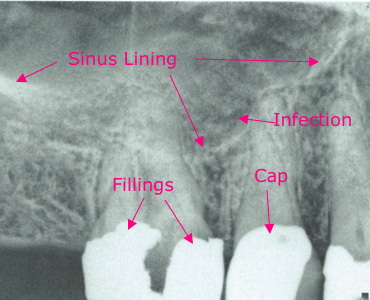 I had two cases where tooth infections or abscess appeared to be Sinusitis. Dental x-rays initially didn't show anything, but after antibiotic treatment for a sinus infection didn't work a tooth x-ray 8-9 mos. later did show the dark area (infection) expanded.
I had two cases where tooth infections or abscess appeared to be Sinusitis. Dental x-rays initially didn't show anything, but after antibiotic treatment for a sinus infection didn't work a tooth x-ray 8-9 mos. later did show the dark area (infection) expanded.
It looks like the tooth is inside the sinus, but the sinus in wrapped around the tooth.
Can a Sinus Infection Be Caused by a Tooth? | Oral Answers says,
Hupp's Contemporary Oral and Maxillofacial Surgery textbook states, "Periapical or periodontal infections of maxillary posterior teeth may erode superiorly through the floor of the maxillary sinus. Approximately 20% of cases of maxillary sinusitis are odontogenic."
Basically, that's a fancy way of saying that tooth and gum abscesses of the upper back teeth can eat through the bone and invade the maxillary sinus. It further says that about 20% of all maxillary sinus infections are caused by tooth infections, rather than another cause.
Awful smell / taste after root canal:
I had an awful smell coming from what I thought was a drain in my gums from an infected tooth, but after a root canal and that drain healed up I was still getting the taste.
Some posts said,
"Mucus is a protein, and these bacteria feed on the amino acids cysteine and methionine that are found in proteins. As they feed, anaerobic bacteria produce metabolites that have characteristically noxious smells. One set of smells is related to sulfur compounds. This is the source of that characteristically "rotten egg" smell associated with bad breath secondary to post-nasal drip. Another set of smells is associated with polyamines that produce the classic putrescent odor of decay." Source: TheraBreath.com
Decongestants often have a rebound effect, particularly decongestants that contain benzalkonium. Such decongestants may prove effective initially. However, when the symptoms return within a day or two they will be worse than they originally were.
See The Sinus Flush - MedHelp
The Flip-Turn Sinus Flush is mildly risky, because you have to bend over to do it, preferably in a shower, but you can also do it outside on soft ground, or you can kneel down and lean over a bathtub, or perhaps a plastic basin or tub, with the shower running for steam
If you don't wish to take the risk involved, then at least you may wish to try the Dr.Grossan Hydropulse Nasal Irrigation System. It gently pumps the saline solution into your sinuses, and I don't know if it pumps saline all the way up into the far reaches of your sinuses, because of gravity, but it follows the same line of treatment expressed here.
Treatment of Sinusitis:
Viral sinus infections usually go away on their own within 10 to 14 days. Antibiotics don't work for viral infections. But there are some things you can do at home to help relieve your symptoms:
- Drink plenty of fluids.
- Try over-the-counter pain relievers and decongestant pills to help relieve the pain and pressure in your head and face.
- Put a hot, damp towel or gel pack on your face for 5 to 10 minutes at a time, several times a day.
- Breathe warm, moist air from a steamy shower, a hot bath, or a sink filled with hot water.
- Use saltwater nose drops to help keep the nasal passages open and wash out mucus and bacteria.
Home treatments may help drain mucus from the sinuses and prevent a more serious bacterial or fungal infection.
Bacterial infections can be treated with antibiotics. You will probably feel better in a few days, but some symptoms may last for several weeks. You may need to take the medicine for a longer time if you have chronic sinusitis.
If you have a fungal infection--which is not common--antibiotics won't clear up your sinusitis. With this type of infection, you may need treatment with antifungal medicines, steroid medicines, or surgery.
last updated 20 Apr 2015
|
 Health
Health
 Colds
Colds
 Sinusitis
Sinusitis
 Health
Health
 Colds
Colds
 Sinusitis
Sinusitis
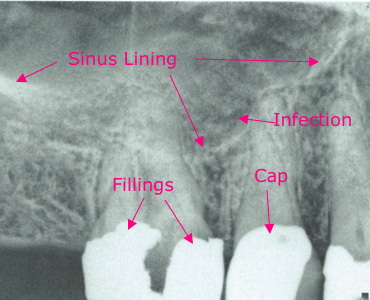 I had two cases where tooth infections or abscess appeared to be Sinusitis. Dental x-rays initially didn't show anything, but after antibiotic treatment for a sinus infection didn't work a tooth x-ray 8-9 mos. later did show the dark area (infection) expanded.
I had two cases where tooth infections or abscess appeared to be Sinusitis. Dental x-rays initially didn't show anything, but after antibiotic treatment for a sinus infection didn't work a tooth x-ray 8-9 mos. later did show the dark area (infection) expanded.